Road to recovery: Cancer in the COVID-19 era
Why cancer must remain a health priority
Just because a cancer has yet to be detected doesn’t mean it isn’t there. As cancer system providers work through backlogs, there will be a near-term surge in cancer diagnoses beyond pre-pandemic levels,1 adding to the strain on the system and putting more lives at risk due to delays in diagnosis and treatment. The effect of delays is also magnified for populations experiencing inequities, who have been hardest hit by the pandemic.
The coming surge in cancer incidence and deaths
 Although trends will vary by jurisdiction and by cancer type, overall cancer diagnoses in Canada are expected to rise in the next couple of years, with the effects lasting until the end of the decade before fully levelling off.2 For example, after a 20% decline in cancer cases during the first wave of the pandemic in 2020, New Brunswick reported a 13% higher incidence for 2020 overall compared to previous years.3
Although trends will vary by jurisdiction and by cancer type, overall cancer diagnoses in Canada are expected to rise in the next couple of years, with the effects lasting until the end of the decade before fully levelling off.2 For example, after a 20% decline in cancer cases during the first wave of the pandemic in 2020, New Brunswick reported a 13% higher incidence for 2020 overall compared to previous years.3
The longer screening and diagnostic delays continue, the higher likelihood that cancers will be discovered later on at a more advanced stage, potentially leading to worse health outcomes for cancer patients.4
Based on early information about the pandemic, one study by McGill University’s Dr. Talia Malagón predicted the possibility of more than 20,000 excess cancer deaths (all types) over the next 10 years. However, that could be reduced to just over 4,000 excess deaths if the cancer system’s diagnostic and treatment capacity is increased by 10% over pre-pandemic levels to meet the growth in demand for those services.2
Spotlight on breast and colorectal cancers
 Modelling studies from OncoSim (a web-based simulation tool co-developed by the Canadian Partnership Against Cancer and Statistics Canada) found that a 40% decrease in breast cancer screening during the first wave of the pandemic could mean that approximately one million fewer screening mammograms were performed in Canada in 2020. As a result of these screening interruptions in 2020, an estimated 3,500 more breast cancer cases than normal may be diagnosed between 2021 and 2023.5 Screening interruptions will also affect the stage of cancer detected at diagnosis, leading to a projected additional 550 late-stage breast cancer diagnoses between 2020 and 2029.5
Modelling studies from OncoSim (a web-based simulation tool co-developed by the Canadian Partnership Against Cancer and Statistics Canada) found that a 40% decrease in breast cancer screening during the first wave of the pandemic could mean that approximately one million fewer screening mammograms were performed in Canada in 2020. As a result of these screening interruptions in 2020, an estimated 3,500 more breast cancer cases than normal may be diagnosed between 2021 and 2023.5 Screening interruptions will also affect the stage of cancer detected at diagnosis, leading to a projected additional 550 late-stage breast cancer diagnoses between 2020 and 2029.5
Similar projections are seen for colorectal cancer. The estimated 40% drop in fecal immunochemical tests (FIT) in 2020 would mean approximately one million fewer colorectal cancer screens were performed in Canada that year. That will lead to an additional 3,200 colorectal cancer cases and 1,200 more advanced-stage cases than normal between 2020 and 2029.5
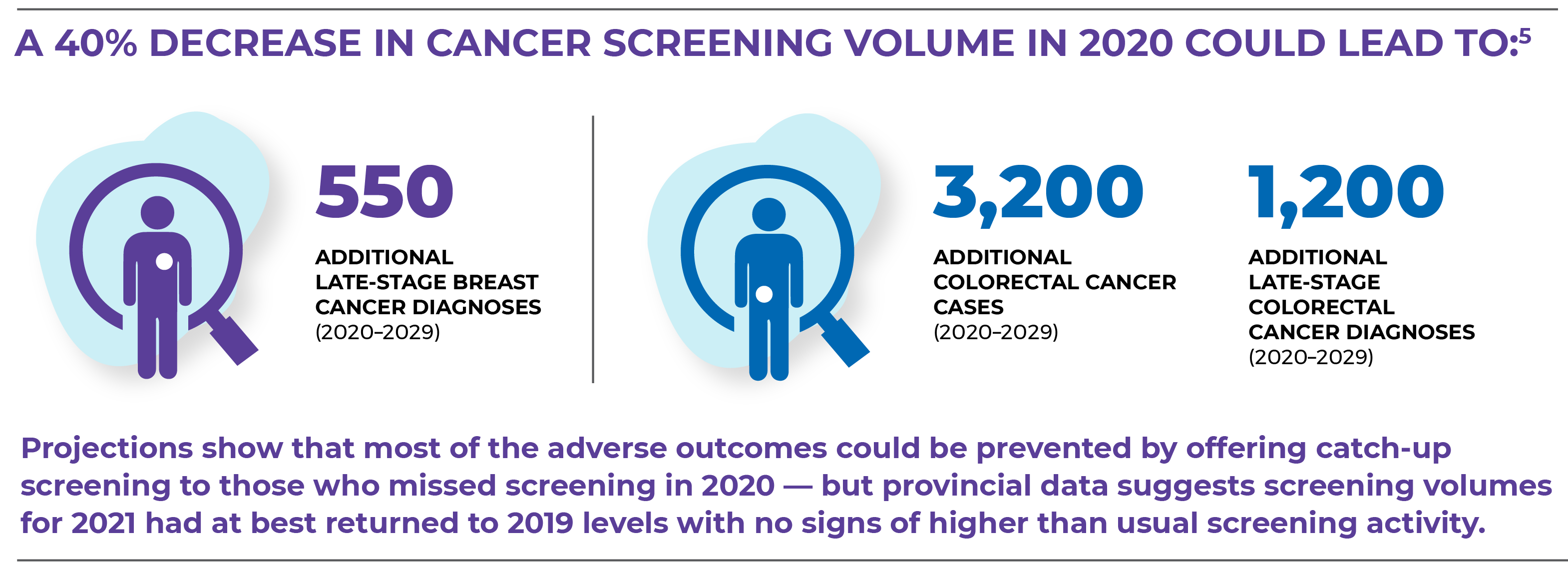
The longer screening is delayed, the more cancers will be detected at later stages, ultimately leading to more cancer deaths that could have been avoided.
The upshot of these projections is clear: many lives could be saved by accelerating a build-up of system capacity to screen, diagnose and treat cancer patients. That requires policymakers and health system players to take action now across several key areas of focus.
- Eskander A, Li Q, Yu J, Hallet J, Coburn NG, Dare A, et al. Incident cancer detection during the COVID-19 pandemic. JNCCN. 2022;20(3).
- Malagón T, Yong JHE, Tope P, Miller Jr. WH, Franco EL. Predicted long-term impact of COVID-19 pandemic-related care delays on cancer mortality in Canada. Cancer Epidemiology. 2021;150(8):1244-54.
- Provincial data submission: New Brunswick Provincial Cancer Registry, New Brunswick Cancer Network, New Brunswick Department of Health.
- Parmar A, Eskander A, Sander B, Irish JC, Chan KKW. Impact of cancer surgery slowdowns on patient survival during the COVID-19 pandemic: a microsimulation modelling study. CMAJ. 2022; 194(11):e408-14.
- Projections obtained from OncoSim, a cancer microsimulation model co-developed by Statistics Canada and the Canadian Partnership Against Cancer.
